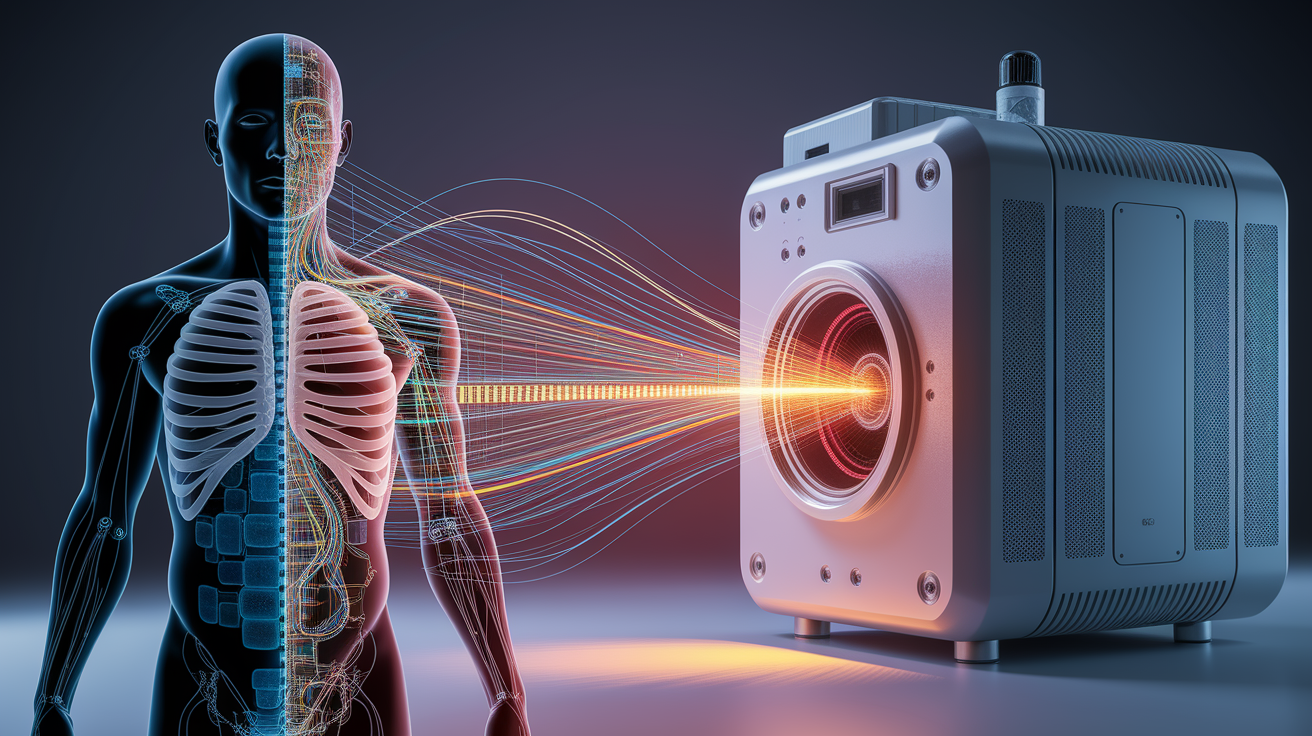
Quick Answer: X-ray machines work by sending a controlled beam of high-energy electromagnetic radiation through the body. Different tissues absorb this radiation differently, and detectors capture the remaining beam to create detailed medical images. Bones appear white because they stop more X-rays, while softer tissues let more of the beam pass through, creating varying shades on the image.
X-Ray Inside Out: A First Glimpse into Image Creation
When you have an X-ray taken, you’re essentially posing in front of a camera that “sees” using invisible light—light so energetic it can pass through skin and muscle but struggles with dense bone. This form of electromagnetic radiation is directed through your body in a way that makes internal structures visible.
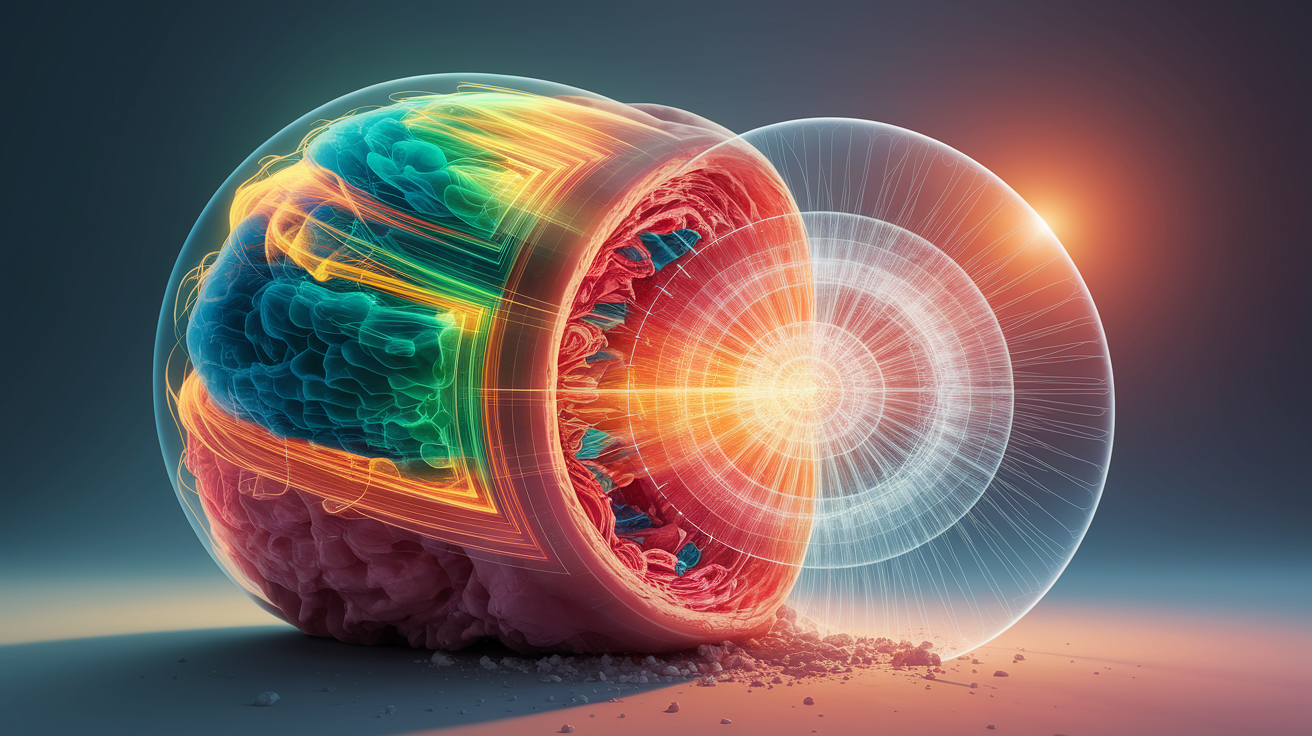
The central idea: different tissues have different densities and compositions. Dense bone blocks much of the X-ray beam, making it appear bright on the final image. Softer tissues allow more X-rays to hit the detector, producing darker areas. This interplay of light and shadow forms the basis of radiographic imaging.
Inside the X-Ray Tube: Generating the Beam
At the heart of every X-ray machine is an X-ray tube—a small vacuum tube where electrons are generated and accelerated. Three important components make this possible:
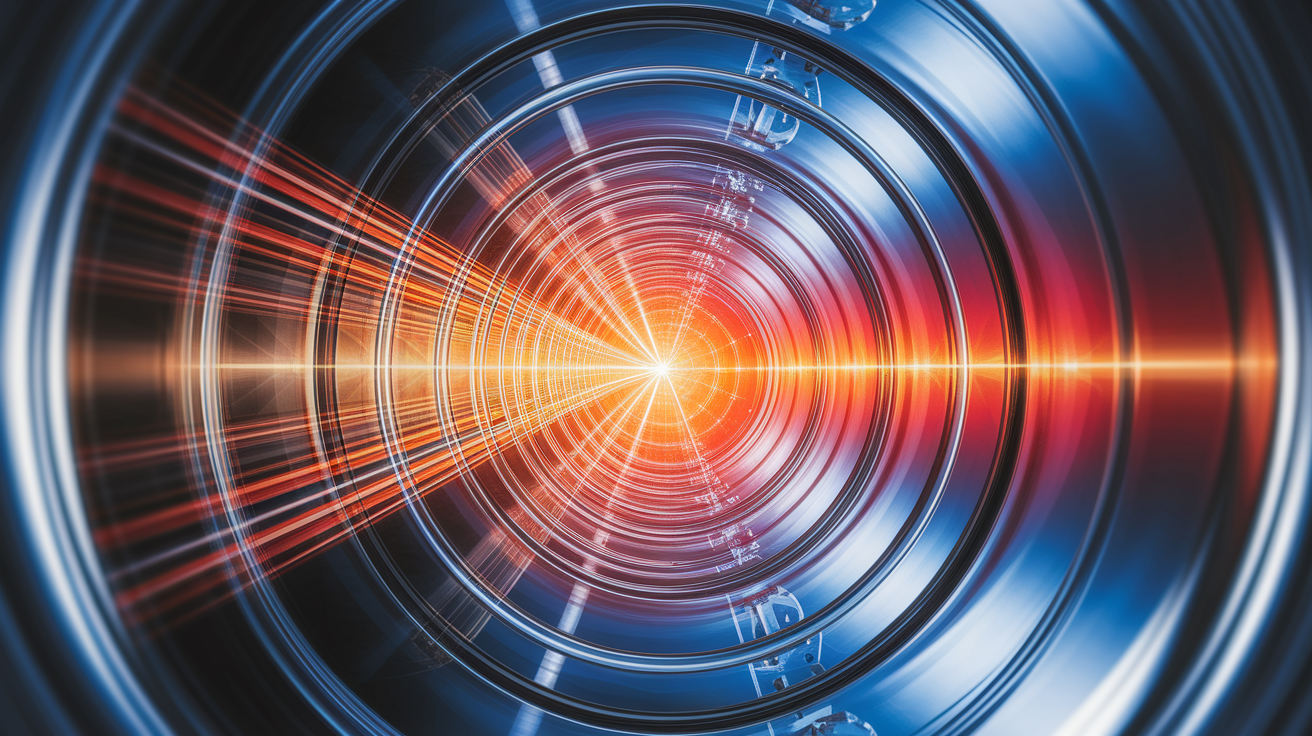
- Cathode: A heated tungsten filament emits electrons through thermionic emission.
- High Voltage Supply: This accelerates the electrons into a speeding electron beam toward the anode.
- Anode with Tungsten Target: When electrons strike the tungsten target, they rapidly decelerate, releasing photons.
Remarkably, only about 1% of the electron energy becomes X-ray photons—most turns into heat. Two main mechanisms produce these photons:
- Bremsstrahlung radiation: Continuous range of energies from electron “braking” near atomic nuclei.
- Characteristic radiation: Discrete energy photons emitted when inner-shell electrons in tungsten are replaced by outer-shell electrons.
From Body to Detector: Building the Image
The beam leaves the X-ray tube and travels toward the patient. As it passes through the body, it experiences beam attenuation—a decrease in intensity due to absorption and scattering.
After passing through the patient:
- Much of the information about internal structures is now encoded in the remaining photons.
- An image receptor—whether a film cassette or a digital detector—captures the exiting photons.
- The differences in photon amounts at various points create the contrast between bright and dark areas.
Bone, being denser, absorbs more radiation, showing up bright. Soft tissue lets more photons through, which the detector notes as darker regions.
Tweaking the Beam: Energy Spectra and Controls
Operators adjust beam properties through settings such as kilovoltage peak (kVp) and milliamperes-seconds (mAs):

- kVp settings: Higher energy photons can penetrate denser body parts but may reduce image contrast if set too high.
- mAs values: Raising this increases the number of photons, brightening the image but also increasing radiation dose.
Filters can remove low-energy photons that do not contribute to image quality but add to exposure. Collimators can limit beam size to the area of interest, reducing scatter radiation and improving clarity.
Advanced Moves: From Single Shots to 3D Scans
Traditional X-rays create flat, 2D images, but modern imaging technology can go further. For example:

- Computed Tomography (CT): Uses a rotating fan-shaped beam and detectors to take many cross-sectional slices, later assembled into detailed 3D images of structures. This significantly enhances diagnostic imaging capabilities.
- Synchrotron sources: Generate extremely intense, tunable X-rays for specialized research and certain advanced imaging applications.
Safety First: Minimizing Radiation Dose
Although X-rays are incredibly useful for medical diagnosis, they involve ionizing radiation, which requires careful management. Safety strategies include:
- Using the lowest acceptable exposure factors for the needed image quality.
- Employing lead aprons or shields to protect sensitive areas of the body.
- Applying beam collimation to limit exposure to the region of interest.
- Standing behind protective barriers for operators.
Radiation dose is a balance: enough to see necessary diagnostic details, but as little as reasonably achievable to protect patients and medical staff.
Bringing Invisible Rays into Clear Focus
X-ray machines are marvels of engineering and physics. They take beams of electromagnetic energy that we can neither see nor feel, direct them precisely through the body, and turn the complex interactions of photons with human tissue into images rich in diagnostic detail. By mastering the interplay between beam creation, tissue absorption, and careful detection, X-ray imaging remains an indispensable pillar of modern medicine—helping doctors peer safely into the hidden landscapes of the human body.