Quick Answer: Broken bones don’t just “patch up” — they go through a remarkable, step-by-step regeneration involving inflammation, tissue building, and fine-tuning until the bone regains its former strength. Most fractures take weeks to months to heal, depending on the injury and individual circumstances.
Building Strong Bonds: Introduction
When you think of a broken bone, the first image that comes to mind might be a cast and a few weeks of rest. But underneath that cast, an astonishing biological repair project is underway. Your skeletal system has a built-in crew of specialist cells ready to orchestrate the bone repair process, working 24/7 to rebuild strength and structure. Understanding this process not only helps you appreciate the marvel inside your body but also shows why proper care and lifestyle choices matter during recovery.

Understanding Bone Healing Pathways
Bone healing can follow two main routes: direct healing and indirect healing.
- Direct (intramembranous) healing: Occurs when bone fragments are perfectly aligned and rigidly stabilized. This allows bone cells to regenerate lamellar bone and the Haversian system almost as if nothing happened — without much remodeling.
- Indirect healing: The more common route, which begins with an inflammatory response, followed by callus formation and eventual bone remodeling. This path involves a temporary “bridge” of cartilage and immature bone that later matures.
Both pathways depend on a healthy vascular supply to deliver oxygen, nutrients, and signaling molecules to the fracture site.
Inflammatory Phase – The Emergency Response
This first phase kicks in immediately after a fracture and can last from hours to a few days. Think of it as a medical triage inside your own body.
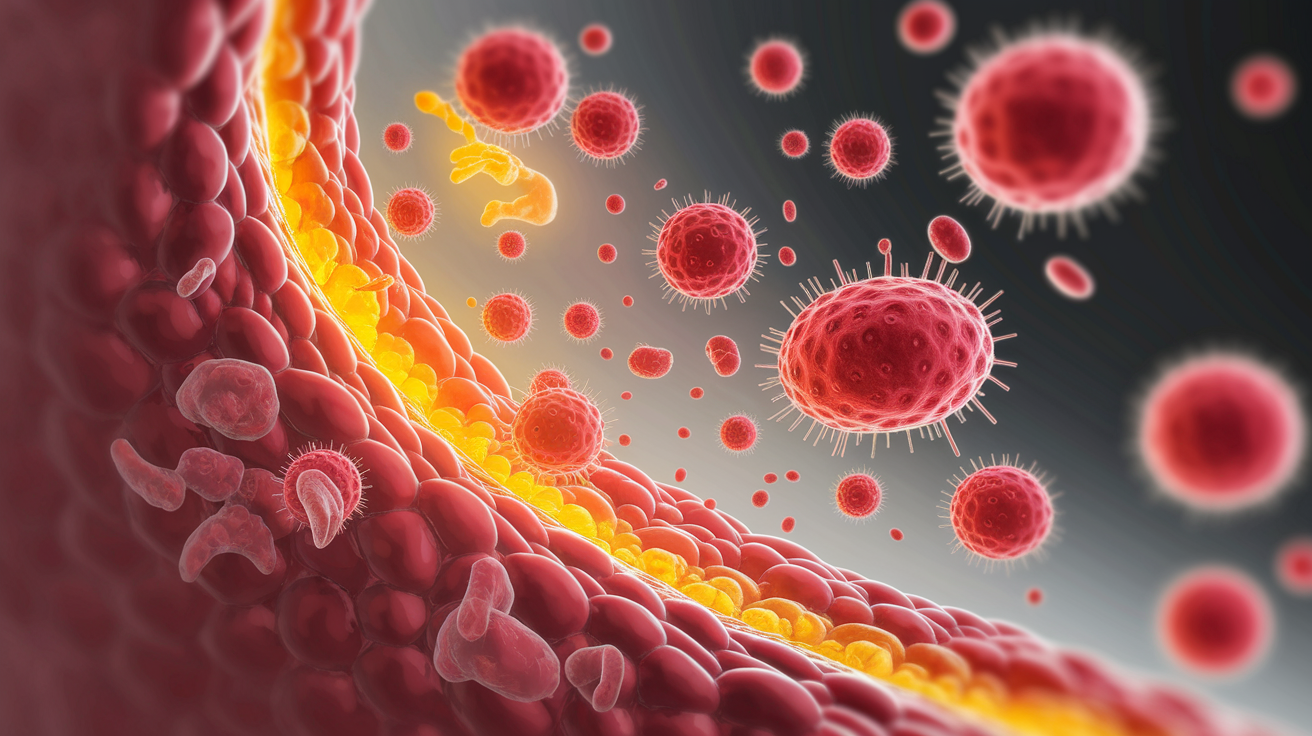
- Hematoma formation: Blood vessels in the bone and periosteum rupture, forming a clot. This hematoma is rich in platelets, cytokines, and growth factors that attract cells to the site.
- Cellular arrival: White blood cells clean up debris while mesenchymal stem cells gather, ready to turn into repair-specialist cells.
- Purpose: Creates a stable, protected environment for healing to begin, much like cordoning off a construction site before work starts.
According to the scientific details on fracture healing, this step primes the site for bone regeneration by initiating both inflammation and vascular changes.
Reparative Phase – Building the Bridge
This is where the real construction work begins, usually lasting several weeks.

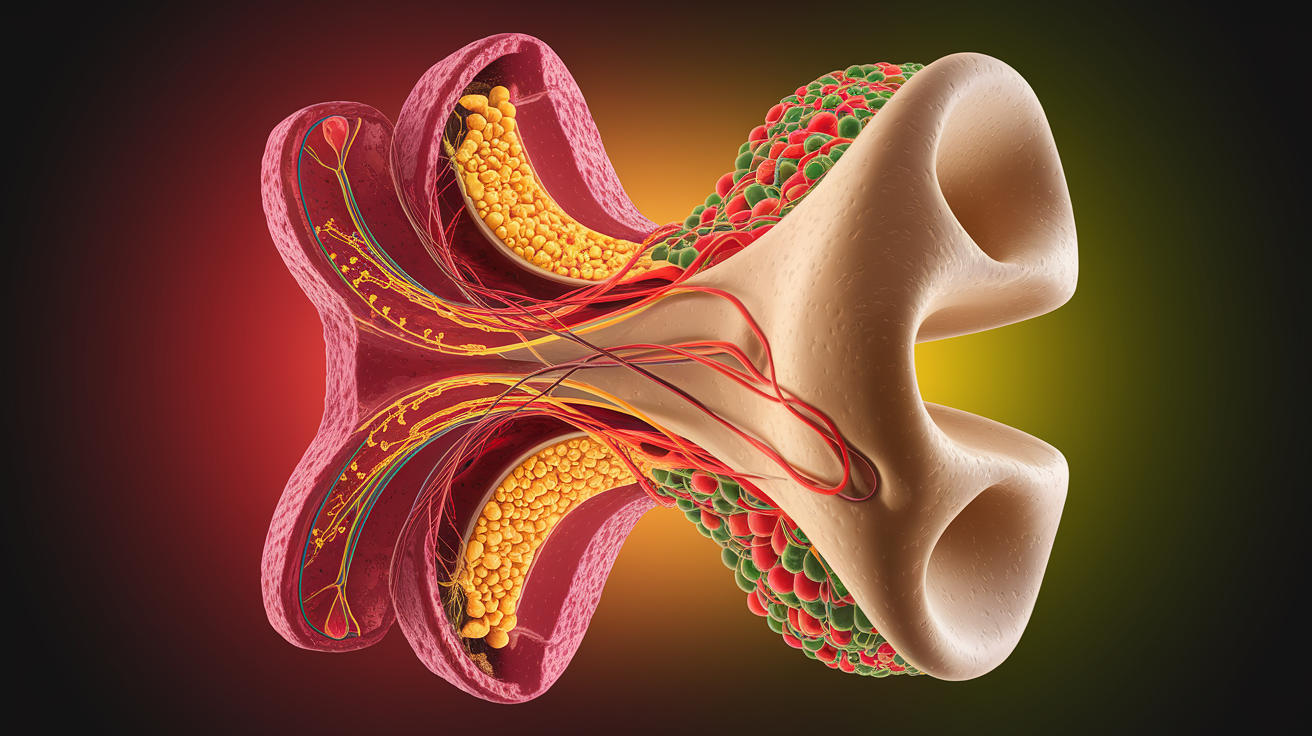
- Soft callus formation: Mesenchymal stem cells become chondroblasts (cartilage-making cells) and osteoblasts (bone-building cells). They lay down a mix of collagen and fibrocartilage that acts as a flexible scaffold between broken ends.
- Hard callus formation: The soft callus undergoes ossification, turning into a hard callus of immature woven bone through a process called endochondral ossification.
- Purpose: The “bridge” now has enough mineralized strength to connect the broken segments, similar to replacing a rope bridge with a sturdy wooden one.
This phase is all about stabilizing the fracture with new bone tissue, though it’s not yet as strong or as organized as the original structure.
Remodeling Phase – Refining the Repair
Now comes the fine carpentry work, which may take months to even years depending on the severity of the fracture and factors such as age and bone involved.

- Osteoclast activity: These cells act like sculptors, resorbing excess bone from the repair zone.
- Osteoblast activity: These master builders lay down organized lamellar bone — the kind found in healthy cortical bone — restoring normal bone density and architecture.
- Result: Bone regains its original strength, shape, and function, often becoming indistinguishable from the surrounding bone tissue.
During this phase, trabecular bone and cortical bone are reshaped to match the original load-bearing demands of the skeletal system.
Key Factors Influencing Healing Success
Healing isn’t just automatic — several factors can speed up or slow down the fracture healing stages.
- Alignment and stability: Precise reduction and proper fixation encourage direct healing. Less stability often means the body takes the indirect healing path.
- Biological environment: Adequate blood supply and healthy periosteum and endosteum tissues are vital for nutrient and cell delivery.
- Patient-related factors: Age, nutrition (especially calcium and vitamin D), overall bone density, and hormonal health matter.
- Lifestyle and health conditions: Smoking, certain medications, infections, and chronic diseases can lead to delayed union or nonunion.
The AAOS fracture healing guide emphasizes the importance of mechanical stability and a healthy biological environment in achieving successful bone union.
Sealing the Repair: Conclusion
Bones may be rigid, but their ability to repair themselves is a dynamic, finely tuned process. From the swift emergency response of the inflammatory phase, to the callus bridge of the reparative phase, and finally to the precise sculpting of remodeling, your body pulls off a complex construction project without you even noticing most of the time. Taking care of your overall health, following medical advice, and allowing the full healing time give nature the best chance to restore your bone’s original strength — a true testament to the resilience of the human body.